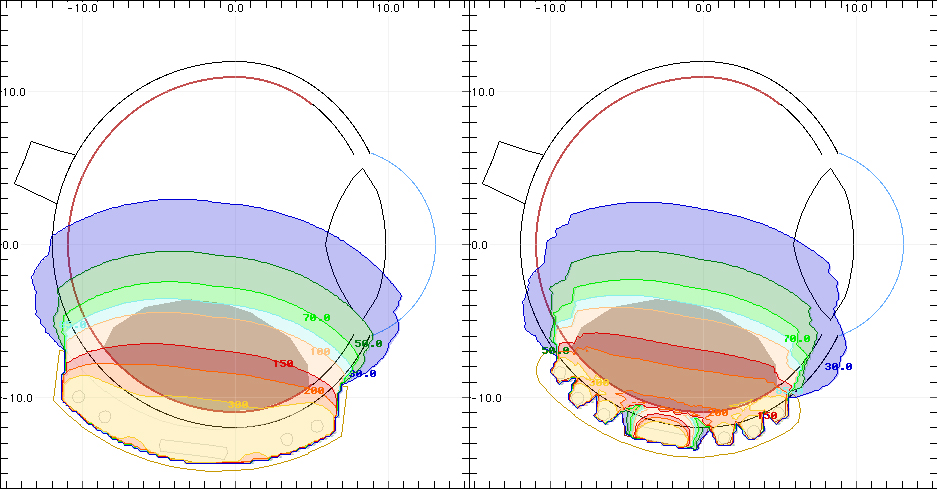
When the anterior of the eye is oblate, the COMS plaque, which conforms only to a 24.6 mm diameter sphere might lift slightly along its posterior edge when sutured anteriorly. This mechanical misfit could result in a tighter than anticipated posterior dosimetric margin (e.g. note the 85 Gy isodose shell) and incomplete dosimetric coverage.
The thinner Eye Physics 3rd generation computer prototyped plaques will soon be available for eyes with diameters from 22 to 26 mm. The Eye Physics plaques will also be available for both spherical and anteriorly oblate eyes and conform to both the spherical posterior and the oblate anterior surfaces of the eye resulting in a near perfect mechanical fit. The size and shape of each patient's eye can be easily determined from CT and/or MR imaging using the Plaque Simulator software.
The most sigificant difference between COMS plaques and Eye Physics plaques is that Eye Physics plaques collimate each radiation source to remove laterally directed primary radiation that does not contribute to the tumor dose. Collimation allows the sources to be moved closer to the sclera resulting in a much thinner plaque, a more homogenous dose distribution between the plaque and the tumor apex, and a reduction in dose to uninvolved retina adjacent to the plaque and to the opposite side of the eye compared to the COMS plaque.
How can this be? Intuitively, we recognize that moving a radiation source closer to the target increases the severity of the "inverse-square" geometric effect resulting in higher entrance dose for a given target dose. This is correct for a single radiation source such as a linac beam, or in the case of eye plaques, a single seed.
Fortunately, eye plaques do not use a single seed. It turns out that the increase in scleral dose relative to tumor apex dose due to increased "inverse-square" is more than offset by the removal of "wasted" lateral radiation from adjacent seeds. A radiation oncology analogy is IMRT compared to a single beam, parallel opposed, 4 fields, etc... IMRT treatments use far more linac monitor units but result in a more homogeneous dose distribution in the target volume and a steeper dose gradient outside the target volume. As an added bonus of sorts, dose to parts of the eye more distal than the tumor apex (e.g. the opposite side of the eye) is also reduced by the increase in the "inverse-square" effect.
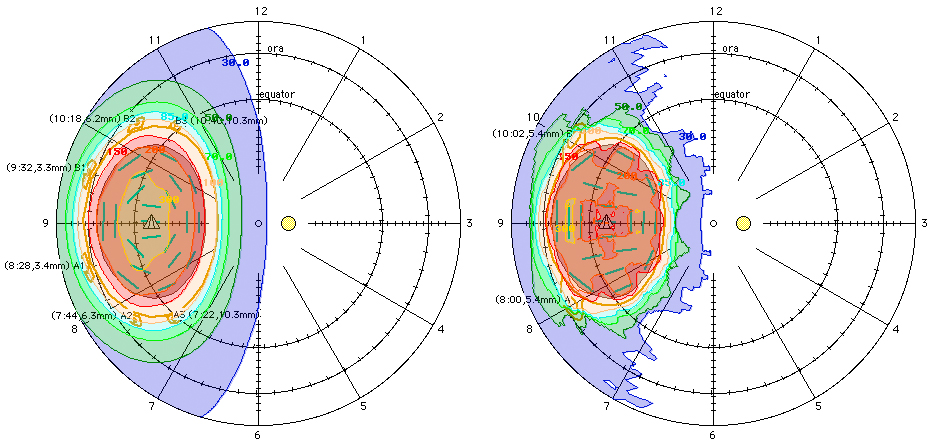
Tumor 14mm circular base x 5mm height, left: COMS-18mm plaque with 21 seeds, right: Eye Physics 3rd generation model 1921-24-0.90 anteriorly oblate plaque with 21 seeds. Isodose lines are in units of Gy. Rx is 85 Gy to tumor apex.

The seeds in a 3rd generation Eye Physics plaque are individually collimated in gold slots. The slot are deeper near the center of the plaque in order to improve dose homogeneity. Slots near the peripheral edge of the plaque are shallower in order to assure homogeneous coverage to the physical edge of the plaque without having to use seeds of different strengths.
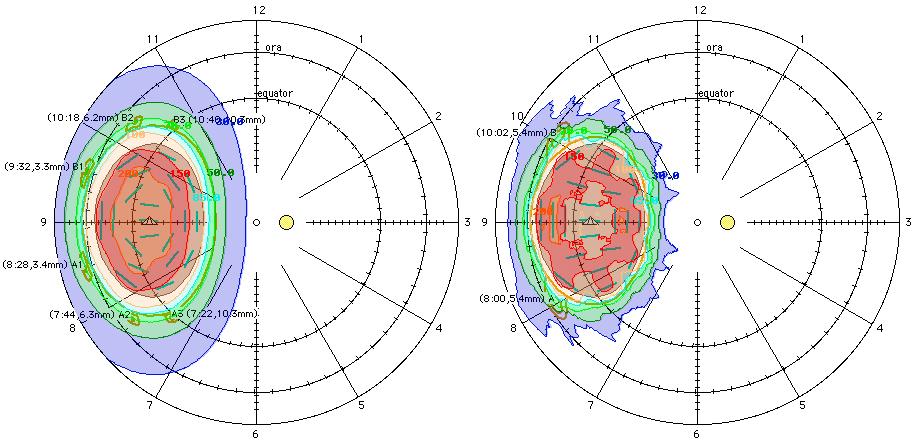
Compare the portion of the eye enclosed within the 200 Gy and 30 Gy isodose lines. The Eye Physics plaque (on the right) produces a more homogeneous dose distribution in the target volume and a steeper gradient outside the plaque perimeter.
The Plaque Simulator software provides precise suture eyelet coordinates to assist the surgeon in placing the plaque at the planned location on the eye.